Most Viewed Pages
- Resin Transfer User Manual
- 1984 Honda Xr350r Repair Manual
- Ktm Sx 125 2018 Repair Manual
- Cat 246b Operators Manual
- Ordinary Differential Equations Solutions Manual James
- Ajax Laundry Manuals
- Aprilia Sport City Cube 300 2008 Manual
- Hesston Model 1160 Parts Manual
- Honda Cb 750 F2 Manual
- Chito Ryu Yoshukai Manual
- Cost Accounting Horngren 6th Edition Solution Manual
- Animec Blood Warmer Service Manual
- Icai Practice Manual For Ipcc Accounts
- Piaggio B 125 2002 Manuals
- Rational Scc 62 Service Manual
- Ktm 85 Sx 2012 Repair Manual
- Vn Commodore Fuel Pump Manual
- Lincoln Ls Repair Manual 2017
- Kubota T L3600 Manual
- White Rogers Thermostat Manual 1f79
- Ingersoll Rand Ssr 15 100 Intellisys Manual
- Wiley Managerial Accounting 6th Solution Manual
Study Guide For Endocrine Disorders
30.01.2020by admin
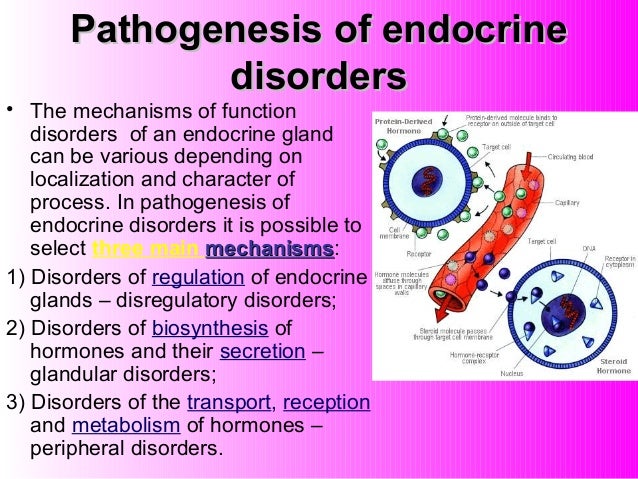
Endocrine system. Problems with the endocrine system occur when there is too little production or excess production of hormones. The onset of endocrine disorders can appear suddenly and be life-threatening, or can appear gradually. Pituitary Gland The pituitary gland is located in the center of the skull at the base of the brain in an area called the sella turcica. The anterior lobe, or adenohypophysis, secretes hormones that stimulate the thyroid gland, adrenal cortex, and the gonads. Growth hormone and prolactin are produced by the anterior pituitary gland. The posterior pituitary produces vasopressin or antidiuretic hormone and oxytocin.
The neurohypophysis, the posterior portion of the pituitary gland, stores hormones produced by the hypothalamus. The hypothalamus shares a circulatory system with the anterior pituitary gland.
This system of nerve fibers connects the hypothalamus to the posterior pituitary and controls how the central nervous system and endocrine system regulate homeostasis of the body. Other functions of the pituitary gland include development of the gonads, regulation of heart rate and rhythm, and assisting other glands in the endocrine system to secrete their hormones. The diagnosis of pituitary disorders is done by evaluating various hormone levels. Computer tomography (CT) scans, x-rays, and magnetic resonance imaging (MRI) can also identify tumors. Alterations in pituitary function are often reflected as a decrease in pituitary hormone or an increase in pituitary hormone. The sections that follow discuss these problems in greater detail.
Hypopituitarism Hypopituitarism is a disorder in which there is a deficiency of one or more of the hormones produced in the anterior pituitary. Deficiencies in thyroid-stimulating hormone (TSH) and adrenocorticotropic hormone (ACTH) often result in hypotension and can be life-threatening. Other problems that occur when there is a lack of pituitary function are failure to develop secondary sex characteristics associated with a lack of gonadotropins, luteinizing hormone (LH), and follicle-stimulating hormone (FSH). A lack of these hormones is not life-threatening but can alter body image and prevent the client from being able to reproduce. Management of hypopituitarism consists of early diagnosis and treatment with hormone supplementation. Hyperpituitarism Hyperpituitarism is a state that occurs with anterior pituitary tumors or hyperplasia of the pituitary gland. Tumors are the most common reason for hyperpituitarism.
Study Guide For Endocrine System
Women with prolactinomas usually experience anovulation, irregular menses, reduction in sex drive, and lactation. Other signs and symptoms of pituitary tumors include headache, visual disturbances, and altered levels of consciousness.
Gigantism (increased levels of growth hormone in the child) or acromegaly (increased levels of growth hormone in the adult) can also result from hyperpituitarism. Management depends on the type and location of the tumor. Many clients respond well to medical management with bromocriptine mesylate (Parlodel) or cabergoline (Dostinex). These drugs should be given with food to decrease gastrointestinal disturbance.
Pregnant clients should not be prescribed Parlodel. Surgical removal of the tumor can be accomplished by a transsphenoidal approach. This type of surgery is performed by passing an instrument through the sphenoid sinus (see ). Clients return from surgery with nose packing in place. Postoperatively the client should be taught to avoid coughing, sneezing, nose blowing, and bending. Soft toothbrushes should be used for several weeks following surgery.
Study Guide For Endocrine
Any discharge from the nose should be checked for glucose because cerebrospinal leakage can occur. Transsphenoidal surgery for the removal of pituitary tumors. X-ray therapy is sometimes used to shrink the tumor. Radiotherapy, a stereotactic radiation, is generally preferred over external beam radiation because a higher dose of radiation can be delivered to the tumor with less radiation to normal brain structures. Damage to pituitary structures of the brain can occur with this treatment, so the client must be assessed for signs of altered neurological function or brain infections such as meningitis. Disorders of the Posterior Pituitary Gland Two disorders of the posterior pituitary gland are diabetes insipidus and syndrome of inappropriate antidiuretic hormone (SIADH). These problems can be caused by a deficiency or excess of the hormone vasopressin (antidiuretic hormone).
Diabetes Insipidus Diabetes insipidus is a result of either a decrease in antidiuretic hormone synthesis or an inability of the kidneys to respond to ADH. The lack of antidiuretic hormone will result in dehydration with resulting hypotension. The nurse should assess the client’s urine for specific gravity. The normal specific gravity is 1.010–1.030. A client with diabetes insipidus will have a specific gravity of less than 1.010. The diagnosis of diabetes insipidus is confirmed by a 24-hour urine screening for osmolality and a hypertonic saline test. This test is done by administering a normal water load to the client followed by an infusion of hypertonic saline and measuring the urinary output hourly.
This test detects ADH release. A decrease in urinary output is a sign of ADH release. Treatment includes chlorpropamide (Diabinese) or clofibrate (Atromid-S) to increase the action of ADH, or if a severe deficiency in ADH exists, the client can be prescribed ADH in the form of vasopressin either nasally or parenterally. The client should be taught to alternate from one nostril to the other because this medication is irritating to the nasal passages.
Syndrome of Inappropriate Antidiuretic Hormone Syndrome of inappropriate antidiuretic hormone (SIADH) is a disorder of the posterior pituitary gland where vasopressin (ADH) is secreted even when plasma osmolality is normal or low. SIADH, or Schwartz-Barter syndrome, occurs when ADH is secreted in the presence of a low plasma osmolality. This alteration results in increased levels of anti-diuretic hormone. High levels of ADH results in excretion of sodium. The incidence is unknown but might be related to cancers, viral and bacterial pneumonia, lung abscesses, tuberculosis, chronic obstructive pulmonary disease, mycoses, positive pressure ventilators, pneumothorax, brain tumors, head trauma, certain medications, and infectious diseases.

Signs and symptoms include nausea, vomiting, muscle twitching, changes in level of consciousness, and low sodium levels with increased urine sodium. The treatment for SIADH includes fluid restrictions because fluid further dilutes the serum sodium levels, gradual replacement of sodium, and administration of demeclocycline (Declomycin) and intravenous hypertonic sodium.
Copyright © 2020 metricsfullpac.